Cancer treatment is often, fittingly, about the cancer itself. Many treatments try to attack the cancerous cells or at least stimulate a stronger response so that the immune system is better able to fight a tumor.
Article published at www.nocamels.com on July 6, 2021.

ancer treatment is often, fittingly, about the cancer itself. Many treatments try to attack the cancerous cells or at least stimulate a stronger response so that the immune system is better able to fight a tumor.
Israeli company OncoHost takes a different approach. Founded in 2017, OncoHost focuses on the host response to cancer therapy, seeking to personalize and modify care rather than develop new treatments. The company does this by measuring changes in the proteins in a patient’s blood before and after treatment, which helps predict whether or not a patient will respond to the therapy and what proteins are responsible for any resistance.
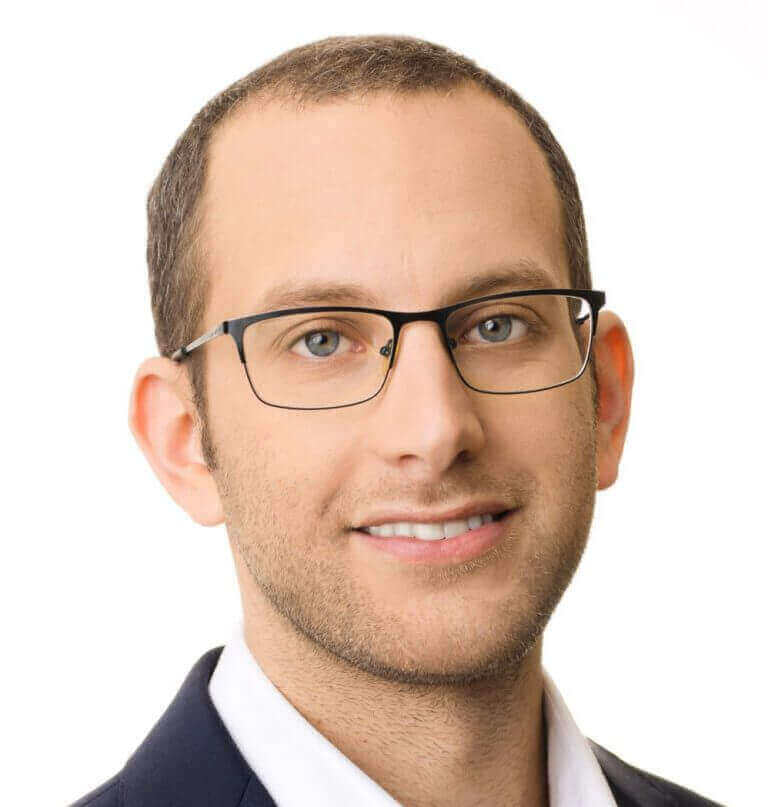
Dr. Ofer Sharon, CEO of OncoHost, shared the significance of this strategy. “Today, what we see is patients are being treated according to protocols. The protocols are kind of a one-size-fits-all approach,” Sharon tells NoCamels. “A 75-year-old lady with lung cancer will be treated exactly the same as a 45-year-old man because we are treating indications rather than patients.”
“The idea with OncoHost is to provide clinicians with tools that will help them to navigate the disease, help them to navigate or manage the treatment better and potentially improve outcomes,” he explains.
Recently, OncoHost announced that it was launching eight clinical trial sites in the United Kingdom in collaboration with the UK’s National Health Service (NHS). At each of these sites, the company will conduct proteomic (protein-based) analysis of advanced-stage melanoma and non-small cell lung cancer patients (NSCLC) who are receiving immunotherapy. This development came on the heels of an $8 million Series B funding round led by OurCrowd.
The new UK sites join many others already operating elsewhere in the world. OncoHost is working with 14 hospitals in Israel, including almost every major cancer center, along with five sites in the US and one in Germany. Several new sites will open soon in the US, Germany, and Denmark, the company says.
“It’s important because cancer is treated similarly but not identically in all countries. So you want to have as many countries as possible to get a really good understanding and really good coverage of the different approaches to treatment,” Sharon says.

An accidental discovery
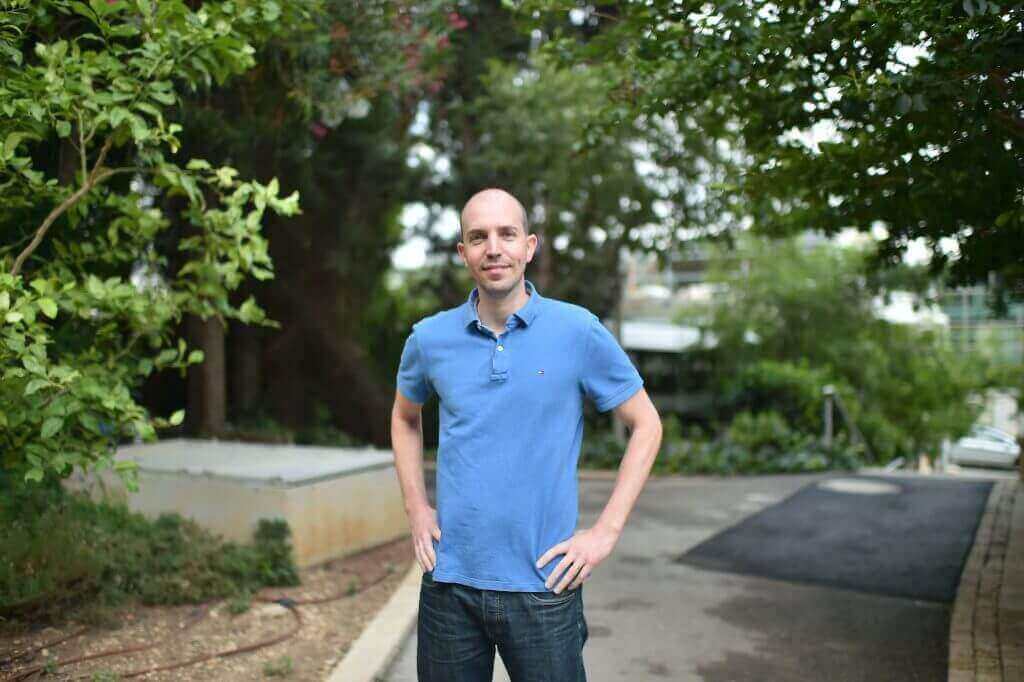
Yuval Shaked, now a professor at the Department of Cell Biology and Cancer Science at the Technion’s Rappaport Faculty of Medicine and the Director of the Technion Integrated Cancer Center (TICC), was working in his lab one day while training at the University of Toronto’s Sunnybrook Health Sciences Centre when he mistakenly added an anti-cancer drug to a petri dish with cancer cells in it. To his surprise, the cancer cells started to die.
As he tried to deduce what had happened, the idea of the “host response” came to his mind. In one petri dish, the anti-cancer drug had been effective, but when testing it in another, it didn’t work. The genetics of the patient and the tumor mattered, of course; but he realized that the associated question, too often neglected, was how the drug treatment itself interacted with the body’s immune cells in complex ways.
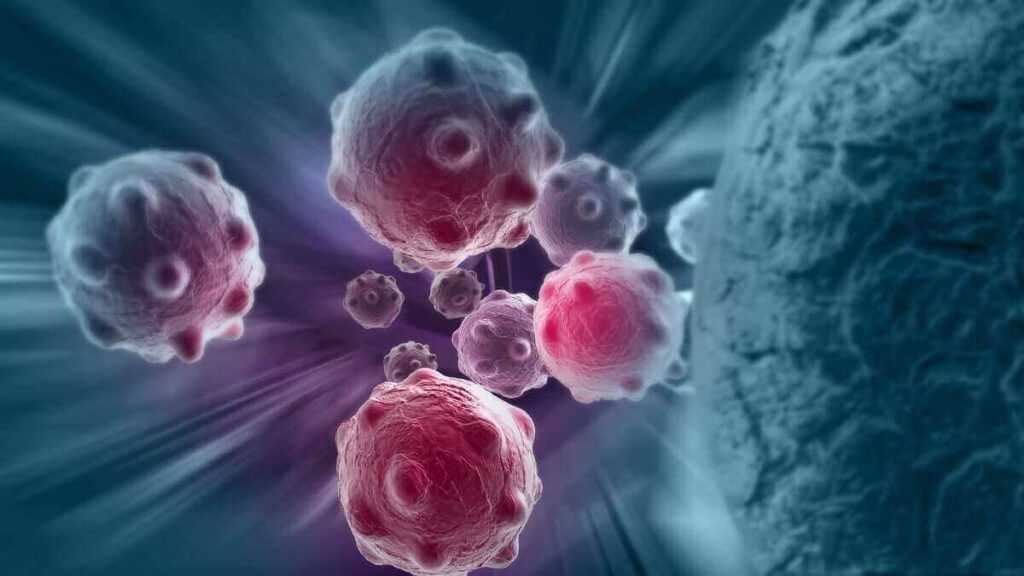
In fact, as years passed and he and others conducted more experiments, Shaked discovered that cancer treatment could even help a tumor grow depending on the host response. Sharon says, “[This] is kind of counterintuitive, right? Our body is working to help the tumor against the treatment.”
He further explains that a tumor is unique because it originates from the patient’s own cells. So for some patients, when the body recognizes the foreign cancer therapy, it may try to support the tumor and fight the treatment.
With these thoughts in mind, Shaked moved to Israel and continued his research until he determined his idea could help launch a company. He co-founded OncoHost and serves as its Chief Scientific Adviser.
Initially, OncoHost intended to identify new drugs or repurpose existing ones. When Sharon came on as CEO a little more than two years ago, he decided the company should go in a different direction. Rather than focus on drug development, OncoHost would become a diagnostic precision oncology company.
The company’s team today reflects this mission. Comprised of both biologists and mathematicians, they work together to combine tumor biology with machine learning tools. Similarly, the Scientific Advisory Board includes clinicians and scientists, offering the both the patient-centered and technical perspectives.
“It’s a hybrid between worlds: mathematics and biology, biology and medicine,” Sharon tells NoCamels.
OncoHost in practice
The team’s first major product, the one currently being tested in clinical trials, is PROphet. The platform combines proteomic analysis with AI and works specifically for predicting responses to immunotherapy treatments, the type of therapy that strengthens the immune system against cancer. When it’s effective, immunotherapy can work extremely well. But for some patients, immunotherapy is ineffectual, and PROphet tries to delineate who falls in which category.
The platform analyzes proteomic changes in blood samples to monitor the dynamics of biological processes induced by the patient (the host) in response to a given cancer therapy.
“Immunotherapy has achieved excellent results in certain situations for several cancers, allowing patients to achieve longer control of their cancer with maintained quality of life and longer survival,” said Dr. David Farrugia, Consultant Medical Oncologist at NHS, and chief investigator of all eight NHS clinical trial sites with OncoHost. “However, success with immunotherapy is not guaranteed in every patient.”
This study, OncoHost’s ongoing trial dubbed PROPHETIC, “is seeking to identify changes in proteins circulating in the blood which may help doctors to choose the best treatment for each patient. I am excited that Gloucestershire Oncology Centre and its research department have this opportunity to contribute to this growing field of research…” said Dr. Farrugia in a statement.

So far, OncoHost’s ongoing PROPHETIC trials have proven successful, including the protein analysis that helps create proteomic profiles. The results have indicated the platform can predict patient responses to therapy with high accuracy.
“Currently, our accuracy level is outperforming every existing biomarker in the market,” Sharon tells NoCamels. “In a way, my assumption is, and what we see since it’s a machine learning-based platform, is that the more we increase the numbers of patients on the platform, the better the prediction capability of the platform is.”
Continued testing and application will be crucial, then, to PROphet’s success going forward. In the coming months, OncoHost plans to launch its first commercial site in the US. The company is currently recruiting employees and building a lab in preparation. In the meantime, clinical trials using PROphet will continue.
The question remains, however, what happens with the information PROphet gathers. OncoHost sends blood test results to a patient’s physician, along with a report detailing the patient’s response predictions and possible next steps.
But sometimes, physicians still may not know exactly how to proceed. While they almost certainly can learn from a patient’s proteomic profile and seem likely to become more attuned to such information as similar technology develops, there are still a lot of unknowns.
“The numbers of clinical decision points that are required from a clinician and the number of options is huge,” Sharon says. “The only way to decide which is the best option is clinical experience and a guess.”
OncoHost’s goal is to help the doctor and patient make this the most informed possible guess. Its clinical trials are currently focused on melanoma and non-small cell lung cancer (NSCLC) and will soon expand to other indications including ovarian cancer, head and neck cancers, and urogenital cancers. This will require resistance mapping for different tumor types and will likely bring in new variables.
OncoHost also has several products in development. One would accelerate the response prediction process before treatment even begins. The other would enable ongoing patient monitoring so a patient knows as soon as possible if their cancer has returned.
Each of these products comes with the same focus — the patient — as part of OncoHost’s unique emphasis on the host response and its efforts to help save lives.