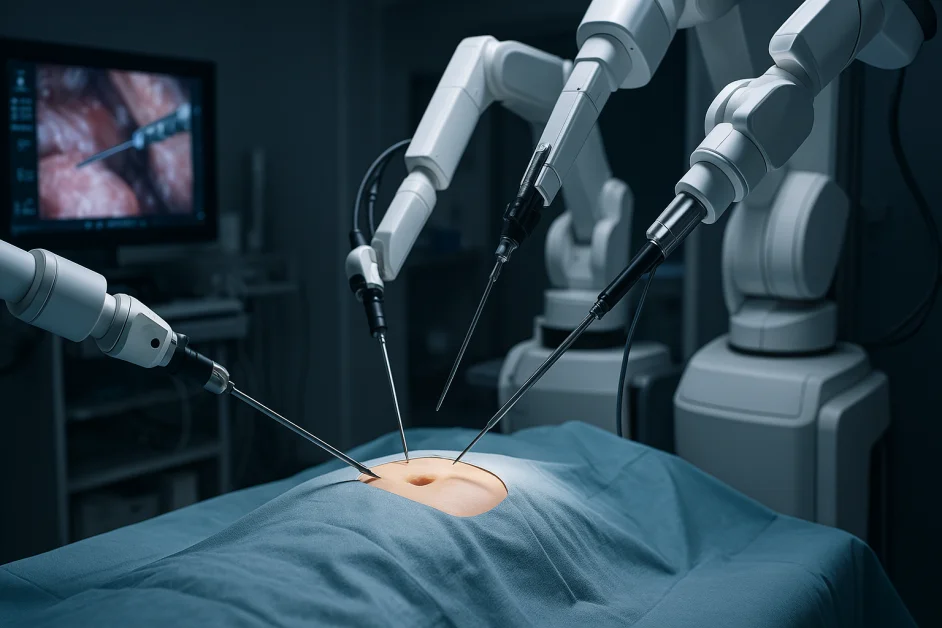
Medical robotics first entered general surgery in the 1980s with laparoscopic tools that enabled minimally invasive procedures, reducing incision size and recovery time. These early systems extended surgeons’ capabilities, transforming the surgical landscape.
Today, artificial intelligence (AI) is ushering in a new era of precision and control in the operating room. Yet despite this progress, robotic systems remain limited to select procedures, leaving most surgeries dependent on traditional methods — and many patients without the benefits of enhanced consistency and outcomes.
As medical technology continues to evolve, how can AI applications in surgical robotics scale to transform healthcare on a broader level?
Fueled by increased robotic VC funding and the digital transformation of the last five years, the robotics industry is seeing fast-tracked market results with no signs of stopping. Earlier this year, Nvidia announced its intent to increase investments in its robot development, signaling a positive shift for the future of robotics. Similar investments in robotics by large-scale players will further advance robotic technology through data collection and machine learning, while providing additional resources and insights.
Surgical robotics industry leaders, such as Intuitive Surgical, Medtronic, and Stryker, have pioneered robotic-assisted surgeries for various procedures. Since introducing its da Vinci system for general surgery in 2000, Intuitive Surgical has continued to iterate its robotic platform to expand its offerings to cardiac, bariatric, gynecology, and thoracic surgeries, among others. With the mass adoption of robotic-assisted surgeries, surgical robotics have consistently been adopted at a faster scale. Between 2012 and 2018 alone, robotic-assisted procedures rose 738% in general surgery.
Looking ahead, surgical robotics have even greater market potential, and are predicted to grow to over $14 billion by 2026 – up from just over $10 billion in 2023. This is mainly due to greater access to robotic surgery procedures, advancements in automation and digital technologies, and new players who aim to deliver cutting-edge medical solutions that harness the power of AI.
Deep Tech Approach
Built on the intersection of disciplines, deep tech merges multidisciplinary technologies such as AI, quantum computing, biotechnology, and robotics to usher in a new era of technology. Startups embracing a deep tech approach in robotic surgery are creating innovative solutions for the future, as can be seen in healthtech development, which can improve patient access to critical medical care. With deep tech development, surgical procedures may become fully automated down the road, requiring minimal surgeon assistance and significantly expanding access to treatment.
Emerging deep tech technologies in surgical robotics can make a lasting global impact. With roughly two-thirds of the worldwide population – 5 billion people – lacking access to surgical treatment, these new modalities, powered by AI, can expand general access and close the surgical care gap.
Fusing AI and Surgical Robotics
AI has innovated and changed how we interact with different technologies and each other. Over the last five years, the transformation brought on by AI has accelerated the development of robotics and created additional applications for AI within different modalities, including robotic surgery.
Here are three essential ways AI is making a fast and profound impact:
1. Embodied AI
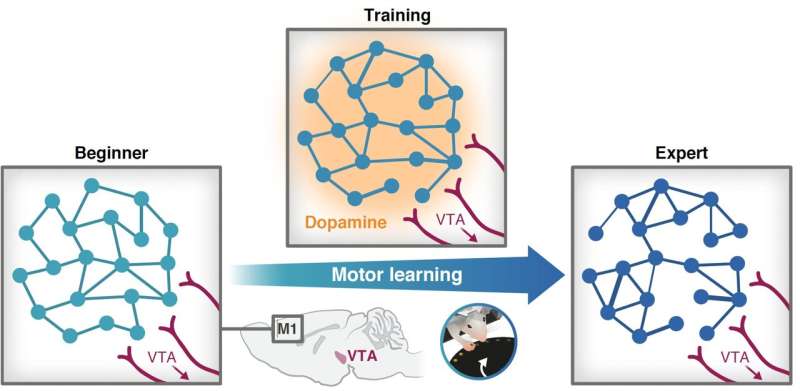
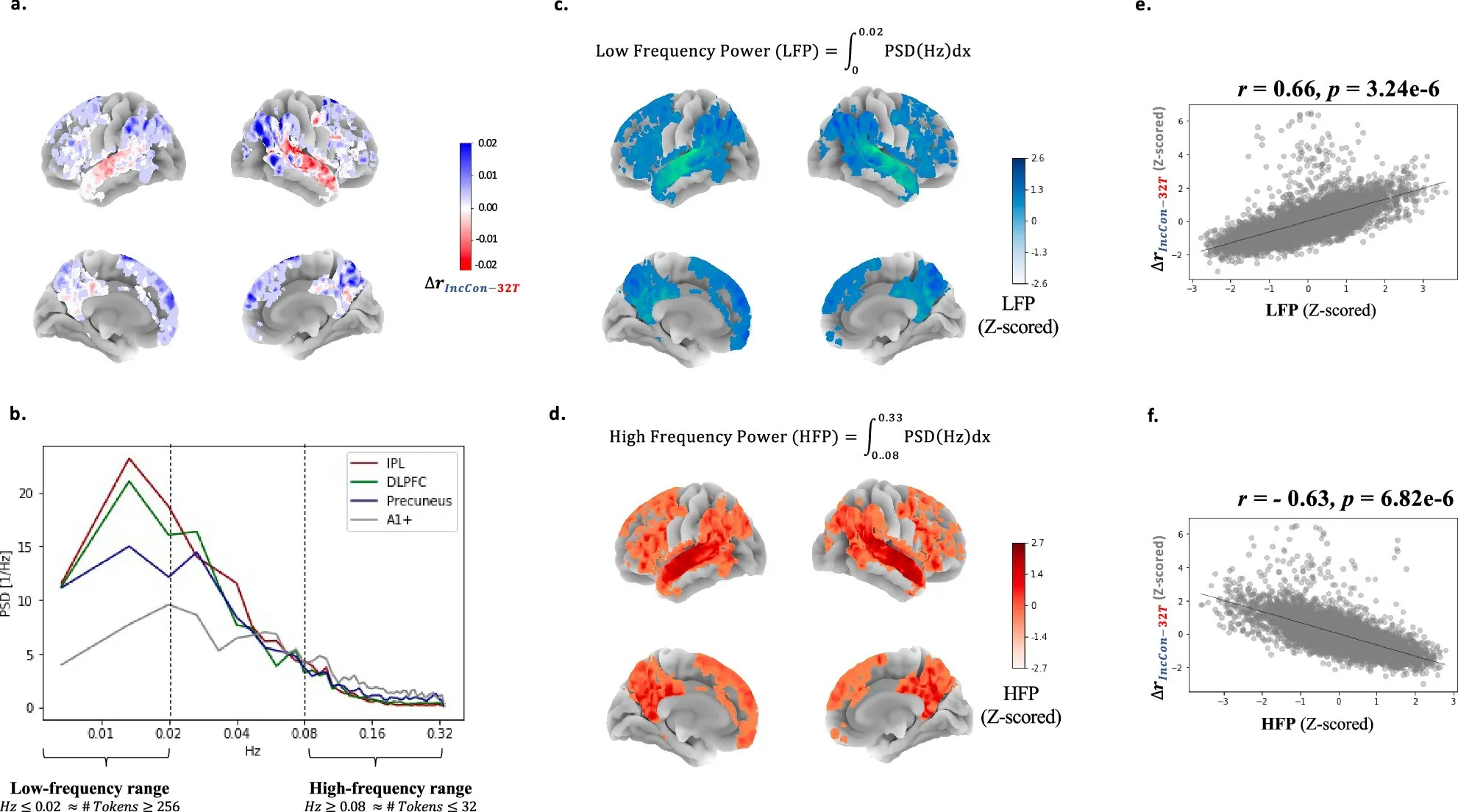
Technology is changing how we interact with our environment and the people around us. Embodied AI, which includes autonomous vehicles and humanoid robots, is the fusion of AI with physical systems to execute complex tasks in real-world settings. When embodied AI is applied to surgical robotics, it has the potential to have long-lasting impacts on enhancing surgical care and improving existing techniques. However, embodied AI requires significant real-world data to develop training simulation models, which are used to train and expand AI capabilities and improve data-driven insights. Until recently, access to large amounts of training data has been somewhat limited; however, as the industry continues to invest in the training and development of AI models, the simulated data pools are growing at a quicker pace and improving embodied AI functionality.
2. Continuous Data Insights and Guidance
AI-based systems can absorb and comprehend large swaths of information in seconds – much faster than the human brain. By training machines on large data sets, data-driven insights can inform surgical decisions before surgeons even set foot in the OR. AI-driven training simulations can significantly benefit surgeons, as training on data sets that are based on thousands of surgeries provide surgeons with trends and techniques to deliver a better patient experience, and also allow them to prepare for and understand the intricacies of rare or complex cases before they face them in the OR. This process can significantly accelerate and shorten the long learning curve surgeons face when training to reach peak surgical performance.
When applied to real-time imaging and visualization technologies, AI-driven data can also enhance surgeons’ decision-making capabilities during operations. By providing surgeons with insights to adjust surgical plans during procedures, AI-based systems can empower surgeons to optimize techniques and approaches in real-time. Through AI-driven imaging systems, surgeons can receive advanced imaging analytics and real-time 3D “maps” of the surgical sites. These augmented overlays can give surgeons expanded insights into the surgical field alongside real-time feedback on their surgical techniques. Robotic surgery platforms are at the forefront of integrating this technology into the OR, with the goal of increasing surgical precision and outcomes.
Furthermore, by providing ongoing feedback post-operation, AI-based systems can provide valuable feedback to surgeons about their performances during procedures – highlighting weaknesses and strengths, and suggesting specific strategies on how to improve them. Such platforms can also recommend new treatment plans based on each patient’s history and the particular procedure’s data analysis, and empower surgeons with additional information that can enhance further treatment. As such, AI platforms have the potential to absorb and adapt surgical feedback throughout the full surgical cycle (before, during, and after) through an AI feedback loop to increase surgeons’ precision and performance.
3. Increased Accuracy and Precision
Individual surgical skills often vary among surgeons due to their access to top-tier opportunities, from program location to surgical mentorship access. For instance, the field of ophthalmology has a steep learning curve. On average, it takes at least 15 years of training and surgical experience to reach peak performance as an ophthalmic surgeon. With a growing aging population and a dwindling number of surgeons, a new solution is needed to reduce the surgeon’s training period and standardize the accuracy and precision of care for all.
In addition to reducing the learning curve for surgeons and allowing them to reach peak performance faster, introducing AI-based platforms into the surgical process can increase accuracy and precision and may improve suboptimal outcomes. Semi-autonomous and increasingly autonomous features in robotic platforms can eliminate the surgeon’s natural hand tremor and improve overall precision and accuracy, thus improving clinical outcomes. In addition, the ability of AI-based systems to recognize unique anatomical structures and provide the exact location for incisions and other surgical steps – especially in complex procedures or anatomical areas – can significantly reduce the rate of surgeon errors by improving spatial awareness of anatomical structures. As such, all surgeons utilizing AI-based systems will be able to provide consistently more precise care.
When incorporated into the surgical process, AI-based robotic platforms provide invaluable insights that can enhance the overall experience for both the patient and the surgeon.
Conclusion
AI will continue to play a significant role in advancing healthcare in the future. Incorporating advanced AI technologies into our healthcare services, such as electronic filing, diagnostics, and health monitoring and tracking, as well as surgical care, is imperative. In doing so, we can improve the overall patient and surgeon experience.
In robotic surgery, AI is expediting the technology’s transformation and patient access to consistent, high-tier treatment. Advancements in robotics, coupled with AI and automation, will continue to usher in new applications, creating a higher level of standardised care and launching healthcare quality and access to new heights.