Israeli health tech startup NeuroKaire, Cofounded by Dr. Daphna Laifenfeld who has a PhD in Medical Science and Molecular Biology from Technion, has rolled out a blood test in the US and Israel that they say can measure the responsiveness of a patient with major depressive disorder to common antidepressants.
This week, NeuroKaine have rolled out a blood test in the US and Israel that they say can measure the responsiveness of a patient with major depressive disorder to common antidepressants.
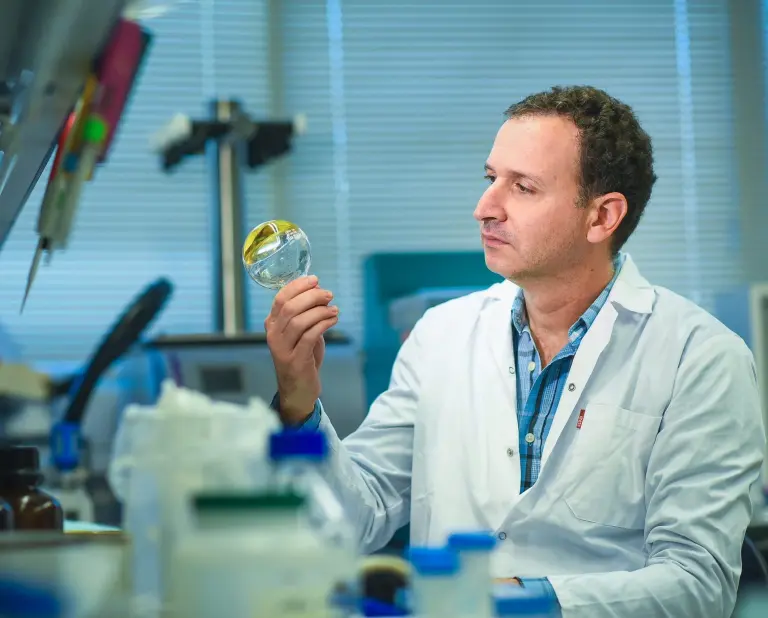
NeuroKaire says its novel, AI-assisted tech uses stem cells to create a brain proxy against which drugs can be tested to find the best one.
Depression is one of the most common forms of mental disorder, affecting more than 330 million people worldwide. Treatment methods rely primarily on a taxing trial-and-error process to find the right prescription drug, which can take years.
In Israel, the psychological toll of 23 months of war and counting has made the need for effective mental health treatment felt more than ever.
The blood test, promises to create a platform for personalised treatment of mental disorders. Guided by the test results, clinicians and psychiatrists can determine which treatment is most suited to a particular patient’s condition.
“For far too long, patients with clinical depression have endured a grueling trial-and-error process before finding an effective treatment,” Cohen Solal told The Times of Israel. “Around one-third of the time, a patient improves or recovers from depression when seeking treatment, and around two-thirds of the time, physicians will need to change their medication or dosage multiple times.”
“Typically, the guessing game of identifying the right drug for a patient with clinical depression can take between 12 to 18 months. We are bringing that down to two months,” she claimed.
The blood test began being offered in Israel and the US this week, though the new technology still needs more research and trial data to determine its effectiveness, according to Prof. Mark Weiser, who heads the Psychiatry Department at Sheba Medical Centre.
“NeuroKaire’s unique combination of stem-cell technology, genomics, and AI represents an evolutionary step forward from traditional pharmacogenetics and is promising, but more research needs to be done in large clinical trials with hundreds of patients, comparing the outcomes with those that haven’t taken the test, and further improve results for patients,” Weiser said.
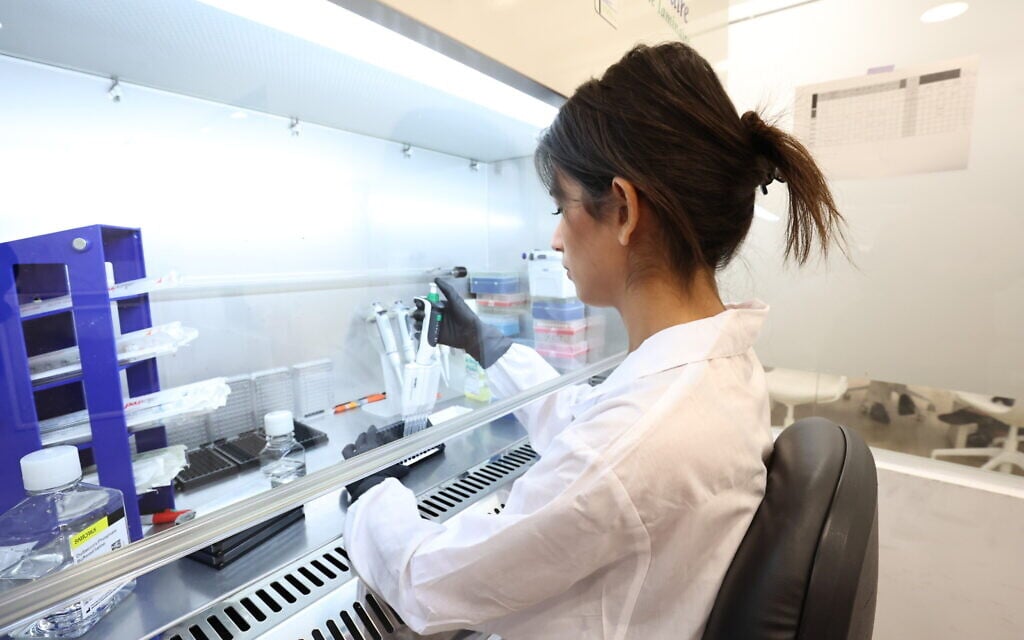
NeuroKaire’s blood-based screening tool, BrightKaire, was recently granted laboratory-developed test regulatory approval from the Centers for Medicare & Medicaid Services in the US, making it the first clinically deployed test based on neurons derived from blood, the startup said.
Cohen Solal and Laifenfeld have decades of academic expertise in brain research and personalised medicine between them. Cohen Solal spent a decade studying psychiatric disorders at Oxford University, University College London and Columbia University. Laifenfeld has worked in brain research at the Technion and Harvard University, and has over 20 years of experience in personalised medicine, including serving as head of precision medicine at Teva Pharmaceuticals Industries.
The two neuroscientists met when Cohen Solal immigrated from the US to Israel in 2017, and they decided to join forces to found NeuroKaire in 2018. The two shared a vision to develop a more precise personalised test that clinicians could use in order to pick the optimal drug therapy for patients with clinical depression.
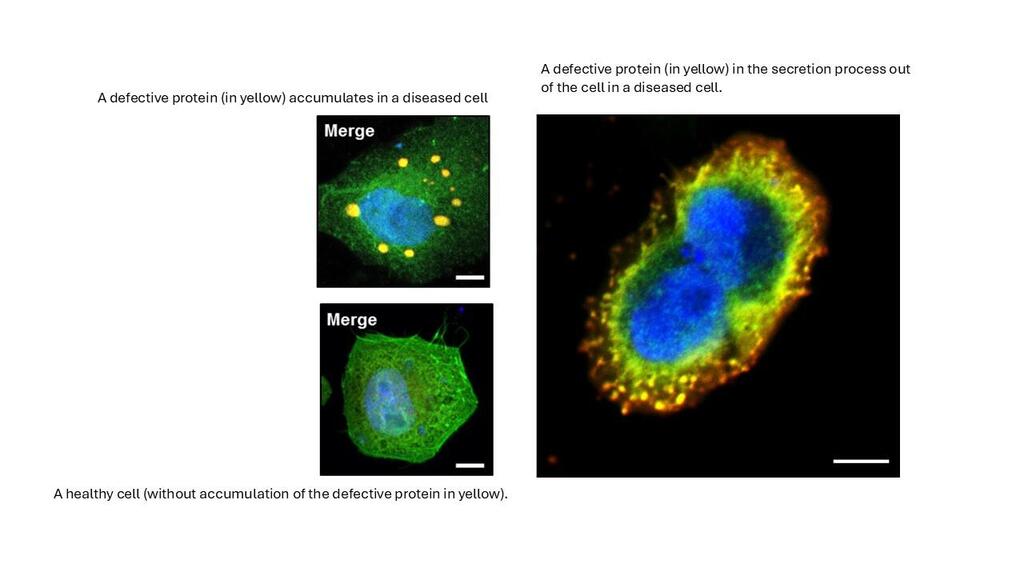
NeuroKaire’s R&D team then turns the stem cells into frontal brain neurons — the brain region most implicated in mental illness and depression — and tests them against 70 different antidepressants, helping to pinpoint the most effective drug or combination therapy for each patient.
Using a proprietary AI platform to analyse personalised data, including a patient’s genetic data, medical history, and microscopic neuronal imaging, the test produces a report detailing the patient’s response to different medications, including the likelihood of side effects.
“Depression is reduced connectivity in the brain, often expressed in a lack of motivation,” Cohen Solal explained. “With our brain in a dish platform, we have a window into the brain and can analyze how well those neurons are connecting or communicating after exposure to antidepressants, and we turn that into a quantitative readout for how strongly a drug has affected connectivity in those samples.”
“Our brain in a dish technology tells you not just if the drug gets past the liver to the brain, but what it does in the brain and whether it works,” Cohen Solal noted.
Cohen Solal said that the startup has validated the technology in clinical trials of the blood-based diagnostic in Israel in collaboration with Sheba Medical Center in Ramat Gan and Geha Mental Health Center in Petah Tikva. In the US, trials were conducted at Jefferson Hospital in Philadelphia and in collaboration with the National Institute of Mental Health. In addition, NeuroKaire has formed partnerships with Israeli biotech companies Clexio and Neurosense.
“In the past two decades, our knowledge of human genetics and brain biology has advanced at an unprecedented pace, but it is still limited,” said Weiser. “The underlying problem is that when a patient comes for treatment, there is no test based on biology as to whether I should prescribe Prozac or a different antidepressant, but it is based on consultation and clinical impressions.”
Weiser said other companies that have developed blood tests based on genes to determine the best drug treatment for depression, were not well-validated.
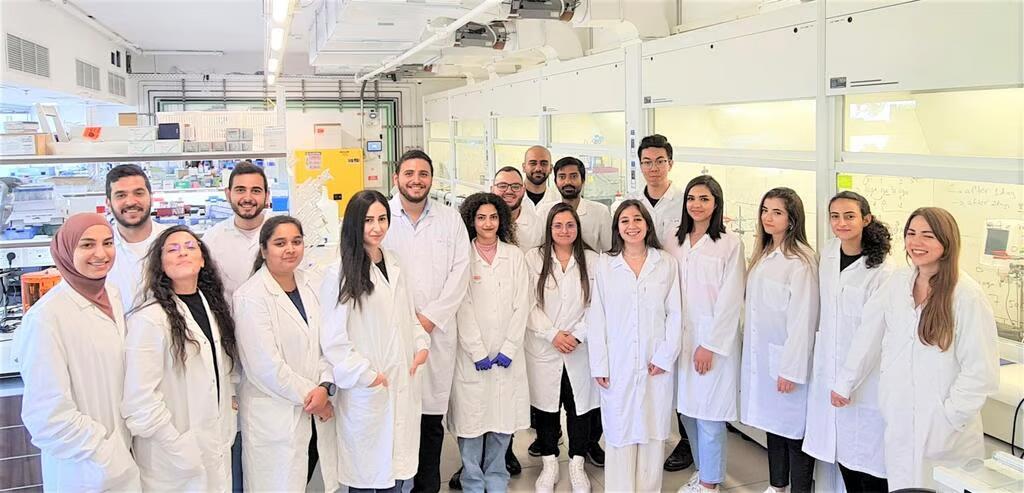
In 2023, NeuroKaire expanded to the US and opened a commercial lab, while its R&D center, employing 25 people, is based in Tel Aviv. To date, the startup has raised $25 million from venture capital investors, including GreyBird Ventures, Meron Capital, Jumpspeed Venture Partners and Sapir Ventures.
“Israel has fantastic life sciences and neuroscience PhDs, which is wonderful for hiring great R&D scientists,” Cohen Solal said. “It’s a mission of ours because of Israel and because of the war to launch this test here as well, and we are very happy to be able to help in this time of need.”
A report published by the State Comptroller’s Office earlier this year found that approximately 3 million Israeli adults may suffer from post-traumatic stress disorder, depression, or anxiety as a direct consequence of the events of the October 7, 2023, Hamas-led massacre in southern Israel and subsequent war in Gaza.
“Many of the drugs overlap for depression and PTSD,” said Cohen Solal. “Physicians can use our technology to help them choose between PTSD medications as well.”
“But in the future, we will specifically be recruiting cohorts of PTSD patients so we can validate it as well in the PTSD setting,” she added.
Cohen Solal said that depression is the first indication, but going forward, tests for other neurological conditions are being planned using the same method.
“NeuroKaire’s mission is to bring precision medicine to the brain,” said Cohen Solal. “Next year, we will be starting our studies in ADHD. That’s going to be our next indication.”